The Importance of Mindfulness
by Tara Duffy
The sun is warm on my skin and a light breeze passes overhead, rustling the branches full of summer leaves. I sit up to take it all in. The dirt is scratchy on my feet, and the towel is warm against my legs. Two dogs run through the water of the lake, best friends who had just met an hour before. A woman suns in her chair, and the dog’s owners sit on the dock with their feet in the water. I hear music and laughter from where I’m sitting, and I smile. The sun glitters on the lake’s surface, and I get up off my towel and walk down toward the water. It’s only May, but the water is already warm. I wade in slowly, and stand in the sun, waist-deep in the water. I am entirely present in this moment, feeling the warm water against my body, my feet in the wet sand, the sun on my face, and the sound of children giggling back on the beach. When I return to my seat, I strike up a conversation with a woman named Sammy, she is visiting her boyfriend who lives in the same town as me. We talk about her family, and how I recently graduated from college with a degree in neuropsychology. She asks the question everyone always asks once you’ve graduated from college. “So, what are you going to do with the rest of your life?” I hesitate, and I respond honestly. “I’m not sure yet.”
With that one question, I’m brought back to reality, the peace of the present moment ended. How do I tell her, “I don’t really know because I truly never expected to graduate from college at all?”
Talking to Sammy on the beach was strange for me because for once, my diagnosis never came up at all. She had no idea that I had inflammation in my spinal cord (transverse myelitis) and a diagnosis of acute disseminated encephalomyelitis (ADEM) or that I still struggle with bladder/bowel dysfunction. She saw a 24-year-old who had recently graduated from college like so many others before her.
It’s been seven years since I first heard the words “transverse myelitis”, but it feels like only yesterday. It was halfway through the cross-country season during my senior year of high school. I had been running ever since I could remember. Apart from the time I had foot surgery, I could never bring myself to stop, until life brought it to a stop against my will. On the verge of one of the biggest transitions that life has to offer, I found myself in the emergency room at Boston Children’s Hospital with the worst case of spinal cord inflammation they had seen to date. I was paralyzed up to my chest, the numbness just beginning to crawl up my fingers when the steroids and IVIG were able to bring it all to a stop.
My sister sat in the emergency room (ER) with me, quizzing me on the parts of the small intestine. Anatomy and Physiology had been my favorite class, and that same teacher was teaching my AP biology class, a class I would never have the chance to finish. During my second week in the hospital, I was given the diagnosis of acute disseminated myelitis, with inflammation present in my brainstem, cervical, and thoracic spine. The doctors said I had enough support at home to do outpatient rehab, but I had to learn how to self-catheterize before leaving the hospital.
Against all odds, I returned to school part-time in February and graduated High School with my class. I started to slip into despair and depression. As my peers went off with dreams of the future, college, and whatever lay beyond, I was left with myself. Myself and transverse myelitis. I hated my body and what it had done to me. I had given up. It was at this time I found a new physical therapist and cognitive behavioral therapist. They helped me enough that I felt confident trying to go to college that fall along with the rest of my peers.
After less than two months, I made the decision to leave college. I was dealing with debilitating pain, bladder/bowel dysfunction, and extreme weakness/fatigue, and trying to fight it was driving me into a hole. After leaving, it was once again me and my diagnosis alone. But this time, I was ready. There would be no running or hiding. I began to meditate and journal, and instead of fighting my pain, I learned to sit with it. This was when I first learned about the psychotherapeutic approach of mindfulness.
Six years later, I was in my final year at The University of New Hampshire’s neuropsychology program, and I’d just completed my senior year internship at Project Walk Boston that summer. This experience filled me with many questions related to those with spinal cord injuries. I had gotten close with two patients with transverse myelitis, one of whom had an extremely positive outlook and believed he would heal and the other who had a bleaker outlook and didn’t believe they would heal. I began to ask myself, “Do these beliefs and thought processes have an effect on physical recovery?” In terms of my own recovery, cognitive restructuring and meditation changed the way I saw myself, my life, and my diagnosis. I wondered if the beliefs and thought processes of others had a similar effect.
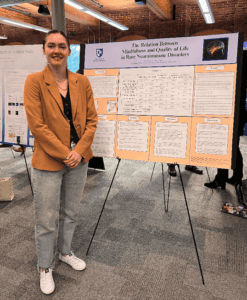
I asked the chair of my department if she would be my supervisor for an independent research study, and I began the literature review in the fall of 2023. After 3 long months of researching and brainstorming, my supervisor finally approved my research question: “Does mindfulness affect the quality of life of people diagnosed with rare neuroimmune disorders?” After applying for and receiving IRB approval, we built the survey and sent it out.
The Five-Facet Mindfulness Questionnaire was used to measure mindfulness, and the Measures of Quality of Life 36-item short-form survey was used to measure quality of life. During a month-long period, a sample of 539 individuals anonymously filled out the electronic survey.
Preliminary findings show that for the majority of the items, mindfulness was positively correlated with higher health-related quality of life (See Pearson Correlation table). Based on these findings, medical providers should encourage patients to practice mindfulness and/or seek mindfulness-based therapies. Additional findings revealed that 63% of respondents reported that it was somewhat to extremely difficult to receive a correct diagnosis, and 59% of respondents said yes when asked if they were aware of mindfulness. When asked how they were aware of mindfulness, the majority reported psychotherapy (39.1% ), a friend and/or family member (32.8%), and/or a physical therapist (25.4%) while only 15% reported from a medical care provider and 17% from a support group. A statistically significant positive correlation of .218 was found between emotional well-being and social functioning.
The majority of respondents reported incomplete to complete motor function (93.6%) and incomplete to complete sensory function (80.1%). age at disease onset was 31.48 (SD=12.209). The average years since diagnosis was 6.0707 (SD=8.34146); Results showed a small difference in paralysis at onset (47.9% tetraplegia and 29.3% paraplegia) compared to current level of paralysis (37.1% tetraplegia and 26% paraplegia). The most common areas of inflammation were the cervical spine (30.6%), thoracic spine (31.9%), and the brainstem (27.5%).
Finally, according to qualitative data from the open-ended part of the survey, the majority of respondents who are not paralyzed report pain, fatigue, and bladder/bowel problems as the biggest factors affecting their quality of life. Respondents also report a lack of community, research, and awareness as negatively affecting their quality of life, especially social functioning.
Respondents report a need for understanding long-term treatment strategies, psychological challenges, and early detection and intervention. Respondents reported feelings of “isolation” due to others not understanding their disease because the symptoms are often invisible. If you feel that you could use more support, consider talking with a mental health provider and find other helpful resources in this presentation from Dr. Meghan Beier of Find Empathy.
Mindfulness
| Observing | Describing | Acting with Awareness | Nonjudging of Inner Experience | Nonreactivity to inner experience | |
| Physical Functioning | .071 | -.025 | -.072 | .104* | .118** |
| Role limitations due physical health | -.104* | 0.026 | .124** | .227** | .063 |
| Role limitations due to emotional health | .193** | .316** | .514** | .332** | .174** |
| Energy/Fatigue | .046 | .217** | .331** | .072 | .014 |
| Emotional wellbeing | .356** | .444** | .482** | .388** | .301** |
| Social functioning | .149** | .171** | .186** | .340** | .249** |
| Pain | .067 | .127** | .044 | .206** | .169** |
| General health | .109* | .160** | .337** | .182** | .052 |
**
. Correlation is significant at the 0.01 level (2-tailed).
*
. Correlation is significant at the 0.05 level (2-tailed).
Listwise N= 539