Acute Flaccid Myelitis: Cause, Diagnosis, and Management
FOR IMMEDIATE RELEASE
Original Publication:
Embargo: December 21, 2020 – 23:30 GMT
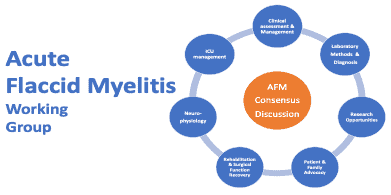
Since 2012, there has been an alarming bi-annual pattern of increases in the number of acute flaccid myelitis (AFM) cases. Although the disorder that we now know of as AFM is not new, the bi-annual spikes, linked to an ordinarily innocuous enterovirus, have raised questions and alarm from a public health perspective. Following the increase in cases in 2018, a group of clinicians and researchers around the United States established The AFM Working Group (AFMWG). This multicentric and multidisciplinary group, led by Dr. Carlos A. Pardo from Johns Hopkins University, was formed and included health care providers, clinicians, and researchers from more than 25 institutions, and patient advocacy groups (such as the Siegel Rare Neuroimmune Association) to address the clinical needs of patients, families, and to support further research. The group began to outline consensus guidelines for improving diagnosis, developing management strategies of clinical concerns found in AFM, coordinating research efforts, and prioritizing research needs. This multi-disciplinary approach of clinicians, scientists, public health agencies, advocacy groups, and families was necessary and innovative. Building consensus from various yet shared experiences of this rare disorder, which at first had no clinical trials or treatment protocols available, has led to a collaborative and comprehensive effort.
This effort has resulted in the first consensus publication of clinical guidance on AFM in the medical journal, The Lancet. Dr. Olwen Murphy, a former James T. Lubin Fellow of the Siegel Rare Neuroimmune Association, led the publication of “Acute flaccid myelitis: cause, diagnosis, and management.” This paper summarizes the critical and substantial work of the AFMWG. From definite to uncertain diagnosis, the authors provide a detailed and comprehensive clinical perspective necessary for medical professionals and families to recognize the symptoms, accurately diagnose, establish acute treatment protocols, as well as near and long-term rehabilitation and recovery strategies for those with AFM.
It is the clinical definition of AFM that this paper sets forth that treating physicians and families should seek to understand when establishing whether or not a child has AFM. The paper breaks down the timeline of an AFM diagnosis from recognition to recovery, outlining recommended protocols for each stage of the diagnosis, and underscores the importance of further studies to aid our understanding of the precise and various disease mechanisms by which an individual ends up with AFM.
It is only through consistent and widely used clinical diagnostic guidelines, treatment plans, and the collection of essential specimens and data that we can begin to understand who will develop AFM after a viral infection and how we can stop it from developing. We can continue to increase awareness, improve on ensuring patients get an accurate diagnosis, and swiftly implement appropriate treatment and rehabilitation strategies to enhance recovery and quality of life of those with AFM.
As the COVID-19 pandemic introduced several emergency public health measures around the world including physical distancing, lockdowns and quarantines, the circulation of other viruses including enteroviruses, the viruses involved as a cause of AFM, decreased dramatically. However, it is expected that once the public health measures around COVID-19 are relaxed and children return to normal school activities in 2021 and 2022, new outbreaks of AFM will emerge. This paper sets up preparedness for such possible outbreaks and focuses on education and awareness for healthcare providers to improve diagnosis and management of AFM.
Members of the AFMWG, including Drs. Carlos Pardo and others, will be presenting about this paper during a Town Hall webinar in January 2021, details will be announced on the SRNA website. They’ll be discussing various details of the paper, their work as a collaborative group, and why the approach they’ve taken to work collaboratively was necessary. They’ll be available to clinicians and families alike to answer questions on the clinical diagnosis and treatment plans for AFM and help advance understanding and research of AFM.
What we now call AFM today was previously considered under the umbrella of transverse myelitis (TM), specifically as a subtype of this disorder. The similarities between the two can be vast, but the two often overlap, from treatment options to long-term management strategies. The more we understand about AFM, the better we will understand other rare neuroimmune disorders like TM, acute disseminated encephalomyelitis (ADEM), MOG antibody disease (MOGAD), neuromyelitis optica spectrum disorder (NMOSD), and optic neuritis (ON).
About The AFM Working Group
The AFM Working Group was established in North America in September 2018 in response to the emergence of AFM as a disabling disease representing a significant public health threat. With a total of 131 group members, it encompasses a wide range of relevant specialties including neurology, pediatrics, infectious diseases, critical care medicine, surgery, and physical medicine & rehabilitation, as well as scientists with expertise in epidemiology, genetics, virology and immunology, and representatives from the patient community. The mission of The AFM Working group is to develop, generate consensus, and share knowledge about the disease for the welfare of individuals diagnosed with AFM in the United States and around the world.
For more information, please visit https://www.acuteflaccidmyelitis.org/.
About SRNA
Siegel Rare Neuroimmune Association was founded 25 years ago by families of loved ones affected by rare neuroimmune disorders. We advocate for, support and educate individuals and their families diagnosed with rare neuroimmune disorders – acute disseminated encephalomyelitis, acute flaccid myelitis, MOG antibody disease, neuromyelitis optica spectrum disorder, optic neuritis and transverse myelitis. We invest in scientific research, therapy development and training of clinician-scientists dedicated to these disorders. We have over 15,000 members and are active in 121 countries. We offer an up-to-date accurate website, resource library of over 300 publications, a patient registry, “Ask the Expert” podcasts, education symposia, the Myelitis Helpline, Quality of Life Family camps, clinician-scientist training Fellowship and a support group network. SRNA is a registered nonprofit organization recognized by the U.S. Internal Revenue Service as a 501(c)(3) non-profit organization with a Guidestar Silver Seal of Transparency.
For more information, please visit https://wearesrna.org/
Other links:
From the CDC
https://www.cdc.gov/acute-flaccid-myelitis/cases-in-us.html
SRNA AFM Hope Ambassadors
https://wearesrna.org/about/hope-ambassadors?fwp_ha_disorder=afm
Contacts:
Carlos A. Pardo, MD ([email protected])
Andrea Salazar, MD ([email protected])