Current Fellows
Sydney Lee, MD
Autoimmune Neurology Fellow, University of Utah
Dr. Lee is a neurologist who received her medical degree from the University of Saskatchewan. She then completed a Residency at The University of Toronto. For her fellowship, she will conduct a study that compares NMOSD preventive treatments in terms of cost and efficacy in preventing disability and preserving patients’ quality of life. First, a group of patients with NMOSD will complete questionnaires, allowing them to identify factors that impact their health and quality of life. This information will then be used to calculate a measurement of quality of life in NMOSD, called a quality-adjusted life year (QALY). They will use economic models to map the course of NMOSD over time and compare the overall cost and effectiveness of each preventative drug. This study will determine the most cost-effective treatment for NMOSD and pave the way toward making these important medications more available to patients.
Rachel Walsh, MD
Clinical Fellow, Boston Children’s Hospital
Dr. Walsh is a pediatric neurologist who received her medical degree from Mercer University School of Medicine. She then completed a Pediatrics and Pediatrics Neurology Residency at Stanford Health Care. For her fellowship, she will evaluate the medical information on a large group of pediatric patients (860 patients anticipated) who presented with symptoms of spinal cord dysfunction and were initially diagnosed with myelitis. She will compare patients based on the underlying cause of their myelitis, including those labeled as idiopathic. The study aims to describe the clinical features and long-term recovery from myelitis amongst the different diagnostic groups as well as better characterize the idiopathic cases. Results are expected to help develop classification systems and definitions, predict outcomes early after myelitis onset, and guide future myelitis studies in children and adolescents.
Haiwen Chen, MD
Pediatric Neurologist, Johns Hopkins School of Medicine
Dr. Chen is a pediatric neurologist and neuroscientist who received her medical degree from the University of Maryland. She then completed a Pediatrics Residency at The Johns Hopkins Hospital in Baltimore, Maryland. For her fellowship, she will work with the neuroimmunology team at the Johns Hopkins School of Medicine to look at how antibodies and immune cells from patients with MOGAD affect brain cells and their connections. Understanding this process may help us understand how MOGAD causes brain and spine dysfunction, allowing us to design better strategies to treat the disease. For example, understanding what part of the immune system may be overactive in MOGAD may allow us to selectively target and suppress that particular part of the immune system to reduce disease.
Past Fellows
Jonathan Galli, MD
Neurologist, The University of Utah
Dr. Galli received his medical degree from the University of Vermont College of Medicine in Burlington, VT, and completed his neurology residency at The University of Utah in Salt Lake City, UT, where he worked with Fellowship mentor, Dr. Clardy. As part of his fellowship training, he conducted research to look for biomarkers in individuals with NMOSD. The research investigated whether individuals have aquaporin4 (AQP4) autoantibodies prior to their symptom onset of NMOSD, and also looked for other inflammatory biomarkers. He hopes the study will help us understand how biomarkers occur over the course of the disorder, which will hopefully help identify predictors of disease development, and ultimately therapeutic targets.
Kyle Blackburn, MD
Assistant Instructor, University of Texas Southwestern
Dr. Blackburn received his medical degree from the University of Kentucky College of Medicine in Lexington, KY, and completed his neurology residency at The University of Texas Southwestern in Dallas, TX, where he worked with his Fellowship mentor, Dr. Greenberg. During his fellowship, he launched a study that collects patient reported outcome measures on adult and pediatric patients with transverse myelitis. The study aims to assess current outcomes in transverse myelitis, and to inform the development of outcome measures for future clinical trials.
Olwen Murphy, MB BCH MRCP
Neuroimmunology Fellow, Johns Hopkins University
Dr. Murphy received her medical degree from University College Dublin in Dublin, Ireland and completed a neurology residency at The Royal College of Physicians in Ireland. She was a James T. Lubin Fellow at the Johns Hopkins Myelopathy and Myelitis Center (formerly the Johns Hopkins Transverse Myelitis Center) in Baltimore, MD, under the mentorship of Dr. Carlos Pardo-Villamizar. Dr. Murphy’s research was on predicting outcomes after a diagnosis of a transverse myelitis using current imaging techniques and spinal fluid analysis. The goal of the research project was to identify patterns or biomarkers that can be used in day-to-day clinical practice to identify benefits from therapies and help make better decisions about care.
Cynthia Wang, MD
Assistant Professor, University of Texas Southwestern
Dr. Cynthia Wang received her medical degree from University of Texas Southwestern Medical Center in Dallas, Texas and completed a pediatrics and pediatric neurology residency at Mott Children’s Hospital, University of Michigan Health System in Ann Arbor, Michigan. Dr. Wang was a James T. Lubin Fellow under the mentorship of Dr. Benjamin Greenberg at The University of Texas Southwestern and Children’s Health. She is now an assistant professor in the departments of Pediatrics and Neurology and Neurotherapeutics at UT Southwestern. Her primary area of interest is immune-mediated brain disorders including ADEM and autoimmune encephalitis. She is conducting a prospective, longitudinal study on acute disseminated encephalomyelitis (ADEM) to identify the clinical characteristics, treatment methods, and follow-up interventions that are associated with better and worse patient-centered outcomes.
Elena Grebenciucova, MD
Instructor of Neurology (MS/Neuroimmunology), Northwestern University, IL
Dr. Grebenciucova received her medical degree from East Carolina University in Greenville, North Carolina. She then completed a neurology residency at the University of Chicago in Chicago, Illinois. Dr. Grebenciucova has been interested in autoimmune disorders of the central nervous system, including rare neuroimmune disorders, since medical school. After residency she completed a Fellowship under the mentorship of Dr. Brenda Banwell at the Perelman School of Medicine of The University of Pennsylvania. Currently she is an Instructor of Neurology (MS/Neuroimmunology) at Northwestern University in Illinois.
Michael Sweeney, MD
Assistant Professor, University of Louisville, KY
Dr. Sweeney completed his undergraduate degree in biological sciences with a focus on neuroscience at Purdue University. Following completion of medical school at the Medical College of Wisconsin, he entered into a combined pediatrics and child neurology residency/fellowship at Cincinnati Children’s Hospital Medical Center. There, he focused his efforts into learning to manage both common and rare neurologic diseases in children. He developed clinical and research interests in immune-mediated neurologic diseases, including multiple sclerosis, neuromyelitis optica, transverse myelitis, optic neuritis and antibody mediated encephalitis. He also worked closely with medical students and residents, demonstrating a strong dedication to education. Dr. Sweeney began his Fellowship at the University of Utah in July 2015 under the mentorship of Dr. Stacey Clardy. Currently he is an Assistant Professor at the University of Louisville in Kentucky.
Allen D. Desena, MD, MPH
Dr. Allen DeSena attended medical school at Loyola-Stritch School of Medicine in Maywood, IL, located in the greater Chicago area. From there, he went on to complete a residency in general pediatrics in New Orleans, LA at the Tulane-Ochsner pediatric program, and he earned his board certification in general pediatrics in 2009. Following his general pediatrics training, he moved to Dallas, TX, where he completed a residency in pediatric neurology at UT-Southwestern Medical Center in conjunction with Children’s Medical Center-Dallas and Parkland Memorial Hospital. During that time, his interest in transverse myelitis and other neuroimmune disorders blossomed, and he pursued further training in those areas. In 2012, he was the recipient of the first James T. Lubin fellowship award from SRNA to pursue a clinical and research career in transverse myelitis and other related disorders mentored by Dr. Benjamin Greenberg, Director of the TM and NMO Centers at UTSW in Dallas. He was the first pediatric neurology fellow to study the rare spectrum of neuro-immunological disorders, with a particular focus on Transverse Myelitis. He was an Assistant Professor in the University of Cincinnati Department of Neurology and Rehabilitation Medicine in Ohio and practiced in Charlotte, NC at Atrium Health.
Participating Institutions
Johns Hopkins Myelopathy and Myelitis Center, Baltimore, MD
Mentor: Carlos Pardo-Villamizar, MD
Bio
Dr. Pardo is Professor of Neurology and Pathology, Division of Neuroimmunology and Neuroinfectious Disorders and Director of the Johns Hopkins Myelitis and Myelopathy Center at Johns Hopkins University School of Medicine in Baltimore, Maryland. He is the principal investigator of the Neuroimmunopathology Laboratory, member of the HIV Neurosciences Research Group and clinical neurologist at the Multiple Sclerosis and Transverse Myelitis Centers at Johns Hopkins Hospital. His clinical specialization is on neuroimmunological and Infectious disorders of the nervous system, with particular focus on multiple sclerosis, transverse myelitis, neurosarcoidosis, and neurological complications of autoimmune disorders.
Contact: [email protected]
Website: Click here
University of Texas Southwestern Medical Center, Dallas, TX
Mentor: Benjamin Greenberg, MD, MHS
Bio
Dr. Benjamin Greenberg received his Bachelor of Arts degree from Johns Hopkins University and his Masters Degree in Molecular Microbiology and Immunology from the Johns Hopkins School of Public Health in Baltimore, Maryland. He attended medical school at Baylor College of Medicine in Houston, Texas. He completed an internship in medicine at Rush Presbyterian-St. Lukes Medical Center in Chicago, Illinois before going on to his residency in neurology at The Johns Hopkins Hospital in Baltimore, MD. He then joined the faculty within the division of neuroimmunology at Hopkins and became the Co-Director of the Transverse Myelitis Center and Director of the Encephalitis Center. In January of 2009 he was recruited to the faculty at the University of Texas Southwestern Medical Center where he was named Director of the new Transverse Myelitis and Neuromyelitis Optica Program. That same year he established the Pediatric Demyelinating Disease Program at Children’s Medical Center Dallas. He now serves as the Director of the Perot Foundation Neurosciences Translational Research Center within the O’Donnell Brain Institute and Vice Chair of Translational Research for the Department of Neurology. Dr. Greenberg is recognized internationally as an expert in rare autoimmune disorders of the central nervous system (e.g., transverse myelitis, neuromyelitis optica spectrum disorder, ADEM and autoimmune encephalitis). He splits his clinical time between seeing both adult and pediatric patients. He routinely consults on the inpatient units of Clements University Hospital, Zale Lipshy, Parkland and Childrens Hospital. His research interests are in both the diagnosis and treatment of transverse myelitis, neuromyelitis optica spectrum disorders, anti-MOG Associated Disorder, ADEM, encephalitis, multiple sclerosis and infections of the nervous system. He is actively involved in developing better ways to diagnose and prognosticate for patients with these disorders. He has led an effort to improve biorepository development and has created uniform protocols for sample handling and analysis. As part of this initiative, his research has identified novel biomarkers that may be able to distinguish between patients with various neurologic disorders. He also coordinates trials that study new treatments to prevent neurologic damage and restore function to those who have already been affected.
Contact: [email protected]
Website: Click here
The Children’s Hospital of Philadelphia, PA
Mentor: Brenda Banwell, MD and Sarah Hopkins, MD, MSPH
Bio
Dr. Brenda Banwell graduated with a degree in medicine from The University of Western Ontario in 1991. She pursued a residency in pediatrics at The Hospital of Western Ontario, University of Western Ontario, from 1991-1994 and a pediatric neurology residency at The Hospital for Sick Children, University of Toronto from 1994-1997. Dr. Banwell then spent two years completing a neuromuscular disease fellowship at the Mayo Clinic, Rochester, Minnesota. In 1999, Dr. Banwell was appointed as an assistant professor of pediatrics (neurology) at the Hospital for Sick Children and University of Toronto. She was promoted to associate professor in 2006 and full professor in 2012. Since July 1, 2012, Dr. Banwell has been Chief of Neurology at The Children’s Hospital of Philadelphia where she holds the Grace R. Loeb Endowed Chair in Neurosciences. . Dr. Banwell’s clinical and research interests are in pediatric multiple sclerosis and other inflammatory brain disorders. Dr. Banwell is the lead Investigator of a 24 site study of acquired demyelination in children, a study that has been continuously funded since 2004. The Canadian Pediatric Demyelinating Disease study now partners with the Children’s Hospital of Philadelphia, and has collaborative research projects with the US Network of MS Centers. A comprehensive clinical, biospecimen, and research-quality MRI database has been established, serving as a core resource to evaluate biomarkers, as well as clinical-radiographic features of TM, ON, ADEM, NMOSD and MS in children. Dr. Banwell also serves as the Chair of the International Pediatric Multiple Sclerosis Study Group and is the Director of the International Medical and Scientific Advisory Board of the Multiple Sclerosis International Federation. In this role, she is involved in advocacy for MS care access, treatment options, and MS information for persons living with MS worldwide. Dr. Banwell has clinical and research expertise in myelin oligodendrocyte glycoprotein (MOG)-related demyelination, as well as autoimmune encephalitis.
Dr. Sarah Hopkins graduated from the University of Arkansas College of Medicine in 2004 and completed residency in pediatrics and neurology at Cincinnati Children’s Hospital Medical Center in 2009, where she remained on faculty for several years. Dr. Hopkins came to The Children’s Hospital of Philadelphia in 2014 and became Section Head of MS and Neuroinflammatory Disorders in 2017. Dr. Hopkins has an interest in inflammatory disorders of the spinal cord and directs the multi-disciplinary Myelitis Clinic at CHOP. She has an interest in acute flaccid myelitis (AFM) and serves as a neurology consultant for the US Centers for Disease Control and Prevention for activities related to AFM Surveillance. She is the site PI for the NIH AFM Natural History Study and the International Pediatric Opsoclonus Myoclonus Ataxia Syndrome Registry. Dr. Hopkins serves as Co-Director of the CHOP/Penn Age Span MS and Neuroinflammatory Disorders Fellowship with Dr. Jennifer Orthmann-Murphy at Penn.
The Demyelinating Disease Program at CHOP is fully integrated with the MS program at the Hospital of the University of Pennsylvania to create an age-span program for demyelinating disorders, and is recognized as a National MS Center of Excellence. The program has a National MS Society funded MS Fellowship program with a well-organized educational mandate.
Contact: [email protected] and [email protected]
Website: Click here
University of Utah, Salt Lake City, UT
Mentor: Stacey L. Clardy, MD, PhD
Bio
Dr. Clardy is both clinical and research faculty in the Division of Neuroimmunology within the Department of Neurology. Her clinical specialization and research focus is in the field of Autoimmune Neurology, which encompasses the evaluation and management of both autoimmune and paraneoplastic disorders of the nervous system. The spectrum of autoimmune and paraneoplastic neurological disorders intersects all traditional neurology subspecialties, including movement disorders, epilepsy, behavioral/cognitive, neuromuscular, autonomic, demyelinating, and neuro-oncologic.
She is devoted to the care of patients affected by antibody-mediated disorders of the nervous system, both autoimmune and paraneoplastic. Areas of Focus include: Autoimmune Encephalitis, Neurosarcoidosis, Neuromyelitis Optica spectrum disorder (NMOSD), Myelin Oligodendrocyte Glycoprotein antibody disease (MOGAD), Stiff Person Syndrome, Myelopathy/Transverse Myelitis, and central nervous system complications of rheumatologic disease.
She established the Autoimmune Neurology Clinic at the University of Utah, one of the few clinics in the United States focused on serving this group of patients. Dr. Clardy is also the Director of the Autoimmune Neurology Fellowship program.
Contact: [email protected] on Twitter as @StaceyLClardy, primarily sharing content about Autoimmune Neurology, and focusing on her role as the Editor of the Neurology Podcast and the Neurology Minute
Website: Click here
Massachusetts General Hospital, Boston, MA
Mentor: Michael Levy, MD, PhD
Bio
Dr. Levy specializes in taking care of patients with neuroimmunologic diseases including multiple sclerosis, transverse myelitis, optic neuritis and neuromyelitis optica. In the laboratory, Dr. Levy’s research focus is on the development of neural stems for regenerative therapy in these diseases. He uses rat and mouse models to test the survival, differentiation and functional capacity of human neural stem cells to improve neurologic function in post-inflammatory conditions. The goal of his laboratory and clinical effort is to translate the basic science stem cell work to a human trial in transverse myelitis and other neuroimmunologic diseases.
Website: Click here
Children’s Hospital Colorado/University of Colorado
Mentor: Teri Schreiner, MD, MPH
Bio
Dr. Schreiner is a neuroimmunology specialist and pediatric neurologist at the University of Colorado and Children’s Hospital Colorado. She sub-specializes in pediatric onset demyelinating disorders of the central nervous system and directs a multi-disciplinary clinic for children with these disorders. Dr. Schreiner treats adult and pediatric patients at both the Rocky Mountain MS Center at the University of Colorado and at Children’s Hospital Colorado.
Dr. Schreiner’s areas of interest include immune-mediated neurologic disease, spinal cord syndromes, including acute flaccid myelitis, quality of life in pediatric patients with demyelinating disease, biomarkers of multiple sclerosis and clinical trials. She is the principal investigator for a novel study, Detection and Risk of Early Multiple Sclerosis (DREAMS), seeking to elucidate risk of future MS in a young population (10-17 years) of first-degree relatives of patients with MS. She participates as site-PI on several multi-center studies funded by federal, foundation, and industry sources.
She has a master’s degree in health policy and administration and, prior to a career in medicine, worked in health care consulting.
Website: Click here
Boston Children’s Hospital
Mentors: Dr. Leslie Benson, Dr. Mark Gorman, Dr. Coral Stredny, and Dr. Margaret Wilson-Murphy
Bios
Dr. Leslie Benson is an attending in the Department of Neurology and the assistant director of the Pediatric Multiple Sclerosis and Related Disorders Program and Pediatric Neuro-Immunology Program at Boston Children’s and an assistant professor of neurology at Harvard Medical School. She received her medical degrees at the University of Colorado Health Sciences Center and completed a pediatric neurology residency and pediatric neuroimmunology fellowship in Boston at Boston Children’s, MassGeneral, and Brigham and Women’s Hospitals. Dr. Benson is directly involved with pediatric AFM, ROHHAD, and demyelinating patient care and research. She directs the multidisciplinary Myelitis Clinic at Boston Children’s Hospital. Her research includes local, national, and international collaborative studies within the field with particular interests in optic neuritis, AFM, and ROHHAD syndrome. She works closely with the 3 other attendings in the neuroimmunology program.
Dr. Mark Gorman established the neuroimmunology program in 2008 and is director. He leads multiple studies on opsoclonus myoclonus ataxia syndrome (OMS) and is involved in studies in demyelinating diseases and autoimmune encephalitis.
Dr. Coral Stredny completed epilepsy and neuroimmunology fellowships. Her primary research interests include autoimmune encephalitis and autoimmune/inflammatory-associated epilepsies, including Rasmussen Encephalitis and FIRES (febrile infection-related epilepsy syndrome), amongst others.
Dr. Margaret Wilson-Murphy‘s primary area of specialty is neuro-infectious disease in addition to neuroimmunology. Her current research is within encephalitis and long term neurologic complications of COVID in children.
Website: Click here
Honoring James T. Lubin
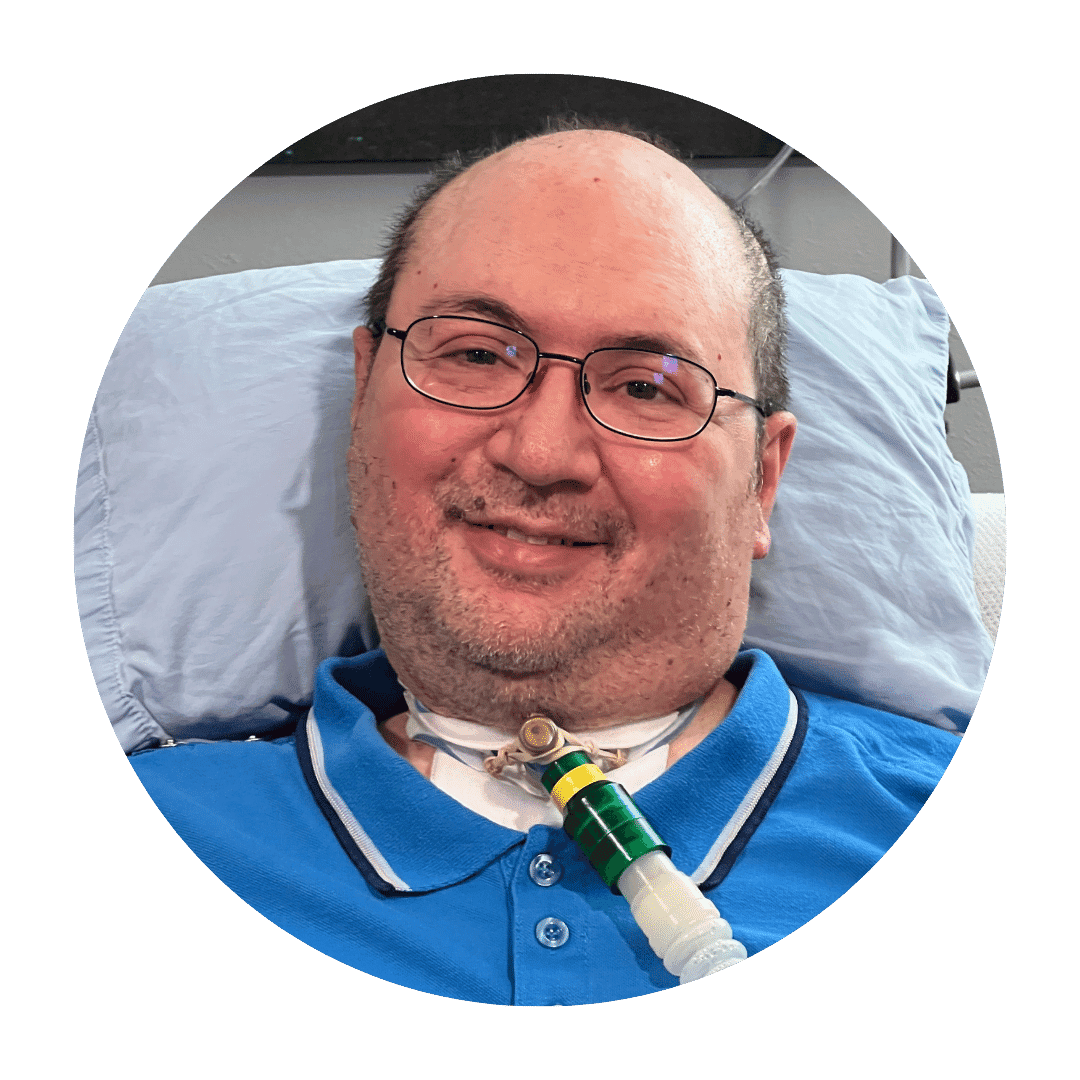
Those who’ve been part of the Siegel Rare Neuroimmune Association, formerly The Transverse Myelitis Association (TMA), for a while know of James T. Lubin. Jim, as he goes by, is one of the founding members of TMA and a member of the Board of Directors of SRNA.
When Jim Lubin was 21 years old, he had a severe attack of TM that rendered him quadriplegic, paralyzed from the neck down, and dependent on a ventilator to breathe. He made the very best out of a difficult situation and relearned how to use computers through the utilization of adaptive technologies.
His skill with computers and his dedication toward connecting and caring for those with disabilities made him a perfect fit. In 1994, he developed the first TMA website and the first transverse myelitis internet club, a list-serve group, where people could find each other, support each other, and learn from each other. Jim has worked for years on the digital aspects of TMA, now SRNA. He gathered a tremendous amount of information on rare neuroimmune disorders and developed and moderated several message boards and forums that helped countless people get their questions answered and connect with others. He has been the backbone of this entire organization.
When asked what drives him to work so hard, despite all the hardships that would likely have discouraged others in his same position, he said the following:
“I just enjoy helping people. When I first set up my disability website, I just went and looked for information and collected it. And when people would reach out to me, even if they didn’t have TM, I’d look for a solution. I’d get thank you cards from people, like a guy who needed a prosthetic ear, and I found a maker for him. There was a need for disability resources to be translated, so I found a translator. There was a need for support groups in other countries, I helped sort that out. And I was never waiting for a cure—I got sick, there’s nothing I did, there’s nothing I could do to stop it. I moved on with my life, I asked, ‘What am I able to do?’ and did that.”
To have made the best of what is an incredibly difficult circumstance and to dedicate one’s life to helping others despite it all is an amazing and honor-worthy choice.
As SRNA’s president Sandy Siegel once wrote, “The James Timothy Lubin Fellowship emanates from our admiration and respect for Jim and our gratitude for all he has accomplished for all of us. Thank you for inspiring the best from each of us, Jim. We love you.”